Gynecomastia is breast enlargement in males due to benign (non-cancerous) breast tissue growth. It is caused by an imbalance between testosterone and estrogen. In other words, there is too much estrogen relative to testosterone. It can be physically uncomfortable, psychologically distressing, and may have a negative impact on self-confidence and body image.
Male breast tissue contains receptors for androgens (like testosterone) and estrogens.1 Most men think of estrogen as an exclusively female hormone, but men also produce it. Normally, the high testosterone levels present in men protect these receptors and inhibit breast tissue development. However, this inhibitory effect is removed if there is either a significant increase in estrogen formation or a significant decrease in testosterone production. The most common causes are detailed below.
Gynecomastia is most common in 1) males going through puberty and 2) males over the age of 50 years.
1) Males going through puberty frequently experience temporary gynecomastia due to the hormonal changes of puberty. This pubertal form resolves in anywhere between 75% to 90% of cases within several weeks to a few years without any medical intervention.2,3
2) Older males typically develop gynecomastia because of hormonal changes due to aging, increased body fat, or certain medications or other substances, all of which will be explained below.
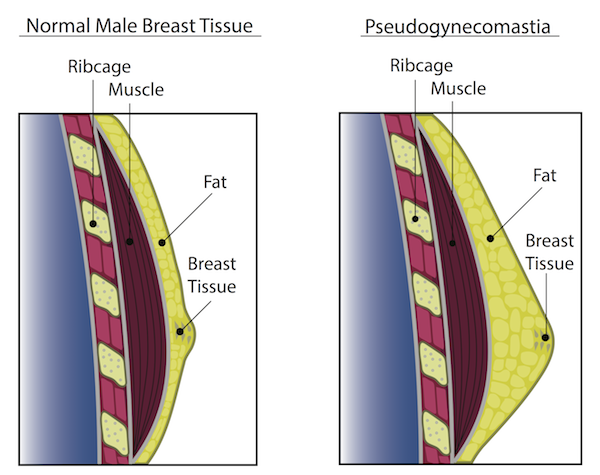
Gynecomastia vs. Pseudogynecomastia
Not all male breast enlargement is gynecomastia. It may also be pseudogynecomastia. From an outward appearance, pseudogynecomastia looks very similar to gynecomastia. In the case of pseudogynecomastia, breast enlargement is due to a buildup of fatty tissue not breast tissue. While the difference may be subtle, the two conditions are treated uniquely, though both are typically treated by surgical removal. Thus, a clinical evaluation by a physician is necessary.
- In the case of gynecomastia, the underlying cause of the hormonal imbalance must be addressed first. Once the hormonal imbalance is addressed, the breast tissue may be excised/cut out by a surgeon, if desired. This breast tissue cannot be suctioned out and has to be removed by surgical excision. It is vital to address the underlying hormonal imbalance prior to surgery because if this imbalance is not resolved, breast tissue may redevelop.
- In the case of pseudogynecomastia, weight loss alone may reduce the fatty buildup. Thus, weight loss should be pursued and is recommended first. If weight loss is not effective, the fat tissue may be liposuctioned out by a surgeon, if desired.
What Causes Gynecomastia?
A number of factors can cause enlarged breasts in men. As mentioned above, the fundamental cause of breast tissue development is either a significant increase in estrogen formation or a decrease in testosterone production. Estrogen stimulates breast tissue growth, so too much estrogen will stimulate breast tissue growth. Too little testosterone prevents testosterone from being able to inhibit breast development.4
The primary factors causing an estrogen/testosterone imbalance include the following:
- Increased body fat – Excessive body fat increases estrogen levels in men, and increased estrogen levels may lead to breast enlargement. Fat tissue contains the enzyme aromatase, which converts androgens like testosterone into estrogen, resulting in the feminization seen in many obese men.5,6
- Primary hypogonadism – Low testosterone levels due to the failure of the testicles to adequately produce enough testosterone upsets the testosterone-estrogen balance.
- Low testosterone due to aging – Testosterone levels decrease with age. The simple hormonal changes with aging may upset the testosterone-estrogen balance and contribute to breast enlargement.
- Chronic liver disease – Liver disease causes circulating estrogen levels to increase because the liver cannot properly metabolize/remove hormones such as estrogen. Also, alcoholic liver disease increases the risk of breast enlargement because ethanol damages the ability of the testes to produce testosterone, and ethanol contains phytoestrogens, which contribute to a higher than optimal estrogen to testosterone ratio.7
- Chronic kidney disease – Kidney disease impairs the body’s ability to remove urea (a common waste product found in urine). High levels of urea suppress testosterone production and damage the testes.8
- Alcoholism – Alcohol damages the testes ability to produce testosterone. Thus, excessive alcohol disrupts the testosterone to estrogen balance. Also, alcohol contains phytoestrogens, which raise the level of estrogens in the body further disrupting the testosterone to estrogen balance.9-11
- Overactive thyroid (hyperthyroidism) – An overactive thyroid increases the conversion of testosterone to estrogen by the aromatase enzyme.12
- Tumors of the testicles, adrenal glands, or pituitary gland – Although rare, tumors of the testicles, adrenal glands, or pituitary gland can produce hormones that disrupt the testosterone-estrogen balance.
- Numerous drugs and/or medications – Numerous drugs and/or medications may also cause breast enlargement. These drugs and medications are detailed below:
Medications
- Certain hormones for prostate cancer – Hormones that block the action of male sex hormones, such as hormones for prostate cancer may induce breast enlargement. Examples include flutamide, finasteride (Proscar, Propecia) and spironolactone (Aldactone).13
- Some cancer treatments (chemotherapy)13
- Certain anti-anxiety, tricyclic antidepressants, ulcer, and heart medications13
Street Drugs
- Anabolic steroids – While anabolic steroids increase testosterone levels above normal, these abnormally high testosterone levels cause more testosterone to be converted into estrogen. In susceptible individuals, this abnormal conversion may disrupt the normal testosterone-estrogen balance.14
- Marijuana – Marijuana interferes with estrogen receptors and acts as a phytoestrogen.15
- Methadone, amphetamines, and heroine
Lastly, environmental exposure to endocrine disrupting chemicals (EDCs), chemicals with weak estrogenic activity, may potentially induce gynecomastia. EDCs can be found in numerous industrial and commercial products such as consumer products, air pollutants, radiation, organochlorine pesticides, plastics, plasticizers, fuels and polycyclic aromatic hydrocarbons. Although not conclusively established, evidence does suggest a link between certain chemicals and breast tissue growth.16-19
Gynecomastia Treatment
The following treatments are broken down into either pubertal or non-pubertal gynecomastia. Puberty induces many transitory hormonal changes that may induce temporary breast enlargement. Thus, the two forms are approached differently. Prior to pursuing any course of treatment, your physician may recommend a mammogram (a simple X-ray picture of the breast) to rule out the rare possibility of breast cancer.20,21
Pubertal
Pubertal gynecomastia is typically not treated. As previously mentioned, between 75% and 90% resolve with time once hormonal changes associated with puberty stabilize.
Non-Pubertal
Gynecomastia not associated with puberty is treated either medically or surgically, with the latter being common and effective. A major factor that should influence the initial treatment is the condition’s duration. Medical treatment may work if started very soon after the start of breast enlargement. However, if breast tissue has been present for some time (usually over 12 months), the breast tissue will likely need to be cut out surgically.
Medical Treatment
Medical treatment is most effective when done very soon after the start of breast enlargement. Medical therapies rarely work if the breast tissue has been present for over 12 months.22 The two most common medications include tamoxifen or clomiphene. Neither medication is FDA approved specifically for gynecomastia, but both medications are used off-label for this condition.23
Tamoxifen
Tamoxifen blocks estrogen receptors within the breast tissue. Thus, it prevents estrogen from exerting its stimulatory effects on breast tissue. Tamoxifen is effective for recent-onset or painful gynecomastia when used in doses of 10-20 mg twice daily.24,25 For recent-onset cases, up to 80% of patients report partial to complete resolution. It is typically used for 3 months before referral to a surgeon. Another drug in the same class as tamoxifen is raloxifene. Raloxifene also blocks estrogen receptors within the breast tissue.
Clomiphene
Clomiphene inhibits estrogen receptors within the breast tissue. Thus, it prevents estrogen from exerting its stimulatory effects on breast tissue. Clomiphene can be administered on a trial basis at a dose of 50-100 mg per day for up to 6 months. In one study, approximately 50% of patients achieve partial reduction in breast size, and approximately 20% of patients noted complete resolution.26
Surgical Treatment
If medical treatment proves ineffective or the condition has been present for over 12 months, the best course of treatment is surgical removal of the breast tissue. As mentioned above, surgical removal involves excising or cutting out the breast tissue. If fatty tissue buildup causes the breast enlargement, the fatty tissue may be removed surgically via liposuction.
Gynecomastia Surgery
Gynecomastia surgeries are performed by plastic surgeons. The surgery is typically an outpatient procedure either in an office operating room (surgical suite) or stand-alone ambulatory center. Outpatient surgery allows a person to return home on the same day that a surgical procedure is performed. The surgery may be performed either under a local or general anesthesia.
Typically, the surgeon cuts an incision along the circumference of the areola in the pigmented portion and directly excises the breast tissue. In the case of fatty tissue buildup, liposuction may also be performed. The objectives of surgical management are 1) to restore the normal male breast contour and 2) to correct deformity of the breast, nipple, or areola.27 Typically, the surgical incision leaves a ½ to 1 inch scar (largely inconspicuous) on the bottom of the areola. The most common incision cut along the bottom circumference of the areola is shown to the right.
Choosing the right surgeon comes down to finding a Board Certified Plastic Surgeon and a member of the American Society of Plastic Surgeons who has significant experience with your type of procedure as well as a Board Certified Anesthesiologist. Additionally, the surgical suite or stand-alone surgical center should be certified by the Joint Commission on Accreditation of Healthcare Organizations. This certification provides you with extra assurance on the highest quality standards of a surgical suite.
Following the surgery, compression garments are applied for at least 2 to 4 weeks. A small amount of blood, injection fluid, and liquefied fat may leak from the incision sites for approximately 24 hours. Drains may or may not be used, depending on the experience of the surgeon and the patient presentation. Drains help to remove excess fluid buildup following the surgery and are removed by the surgeon in a follow-up office visit. Patients typically return to work after 1-2 days and may resume physical activities within a few days. The compression garments are worn discreetly beneath a shirt.
Gynecomastia Surgery Risk
The following are selected potential risks of male breast reduction surgery27:
- Hematoma – Localized collection of blood
- Sensory changes – Reduced areola sensation
- Contour deformity – Depression of the breast
- Breast asymmetry
- Infection
- Painful scar
- Conspicuous scar
- Skin redundancy (excess skin)
Gynecomastia Surgery Cost
First off, most insurance companies will not cover surgery for gynecomastia treatment or male breast reduction on the basis that it is a cosmetic procedure.28-30 Thus, surgical treatment often must be covered out of pocket by the patient.
According to the American Society of Plastic Surgeons, the average surgery in 2013 costs roughly $3,200 for the surgeon fee, although this number can vary widely.
It is important to note, that this figure only represents the surgeon fee. It does not include the 1) anesthesia fee, 2) facility cost (operating room fee) or 3) post-surgery garment cost. Both the anesthesia fee and facility cost may be somewhere in the thousand dollar range each, and the post-surgery garment may cost an additional $100 to $200. Make sure to discuss the cost breakdown upfront, including what services/procedures are covered in the quoted price and what services/procedures are not.
Service/Procedure |
Cost ($) |
| Surgeon Fee | 3200 (Average)30 |
| Anesthesiologist Fee | 500 - 1500 (Estimate) |
| Operating Room Fee | 500 - 1500 (Estimate) |
| Post-Operative Garments | 100 - 250 (Estimate) |
| Total | 4300 - 6450 |
1. Calzada L, Torrs-Calleja J, Martinez JM, Pedrón N. Measurement of androgen and estrogen receptors in breast tissue from subjects with anabolic steroid-dependent gynecomastia. Life Sci. 2001; 69 (13): 1465-9.
2. Shulman DI, Francis GL, Palmert MR, Eugster EA, Lawson Wilkins Pediatric Endocrine Society Drug and Therapeutics Committee. “Use of aromatase inhibitors in children and adolescents with disorders of growth and adolescent development.” Pediatrics 2008; 121 (4): e975–983.
3. Ansstas G, Griffing GT. Gynecomastia Treatment & Management. Medscape Reference. Updated April 17 2014. http://emedicine.medscape.com/article/120858-treatment.
4. Johnson RE, Murad MH. Gynecomastia: pathophysiology, evaluation, and management. Mayo Clinic Proceedings 2009; 84 (11): 1010–1015.
5. Hinson J, Raven P, Chew S. Systems of the Body: The Endocrine System: Basic Science and Clinical Conditions. 2nd Edition. Churchill Livingston Elsevier. 2010.
6. Braunstein GD. Clinical practice. Gynecomastia. N Engl J Med. 2007; 357 (12): 1229-37.
7. Dickson, G. Gynecomastia. American Family Physician 2012; 85 (7): 716–722.
8. Iglesias P, Carrero JJ, Diez JJ. Gonadal dysfunction in men with chronic kidney disease: clinical features, prognostic implications and therapeutic options. Journal of Nephrology 2012; 25 (1): 31–42.
9. Gordon GG, Altman K, Southren AL, Rubin E, Lieber CS. Effect of alcohol (ethanol) administration on sex-hormone metabolism in normal men. N Engl J Med. Oct 1976; 295 (15): 793-797.
10. Bannister P, Losowsky MS, Lowosky MS. Ethanol and hypogonadism. Alcohol. 1987; 22 (3): 213-217.
11. Bartke A. Chronic disturbances of the hypothalamic-pituitary-testicular axis: Effects on sexual behavior and fertility. In: Zakhari S, ed. Alcohol and the Endocrine System. National Institute on Alcohol Abuse and Alcoholism Research Monograph No. 23. NIH Pub. No. 93-3533. Bethesda, MD: National Institutes of Health; 1993.
12. Narula HS, Carlson HE. Gynaecomastia-pathophysiology, diagnosis and treatment. Nat Rev Endocrinol. 2014; 10 (11): 684–698.
13. Anawalt BD, Braunstein, GD, Matsumoto AM. Gynecomastia. Hormone.org. 2011. http://www.hormone.org/questions-and-answers/2011/gynecomastia.
14. Basaria S. Androgen abuse in athletes: detection and consequences. J Clin Endocrinol Metab. 2010; 95 (4): 1533-43.
15. Sauer MA, Rifka SM, Hawks RL, Cutler GB Jr, Loriaux DL. Marijuana: interaction with the estrogen receptor. J Pharmacol Exp Ther. 1983; 224 (2): 404-7.
16. Braunstein GD. Environmental gynecomastia. Endocr Pract. 2008; 14 (4): 409-11.
17. Durmaz E, Ozmert EN, Erkekoglu P, et al. Plasma phthalate levels in pubertal gynecomastia. Pediatrics. 2010; 125 (1): e122-9.
18. Stroheker T, Cabaton N, Nourdin G, et al. Evaluation of anti-androgenic activity of di-(2-ethylhexyl)phthalate. Toxicology. 2005; 208 (1): 115-21.
19. Agency for Toxic Substances and Disease Registry. Toxicological profile for di-(2-ethylhexyl)-phthalate. Atlanta: Department of Health and Human Services, Public Health Service, Agency for Toxic Substances and Disease Registry; 2002. Available from: http://www.atsdr.cdc.gov/toxprofiles/tp9-p.pdf.
20. Volpe CM, Raffetto JD, Collure DW, et al. Unilateral male breast masses: cancer risk and their evaluation and management. Am Surg. Mar 1999; 65 (3): 250-3.
21. Carlson HE. Approach to the patient with gynecomastia. J Clin Endocrinol Metab. Jan 2011; 96 (1): 15-21.
22. Deepinder F, Braunstein GD. Drug-induced gynecomastia: an evidence-based review. Expert opinion on drug safety 2012; 11 (5): 779–795.
23. Bedognetti D, Rubagotti A, Conti G, et al. An open, randomised, multicentre, phase 3 trial comparing the efficacy of two tamoxifen schedules. Eur Urol. 2009.
24. Boccardo F, Rubagotti A, Battaglia M, et al. Evaluation of tamoxifen and anastrozole in the prevention of gynecomastia and breast pain induced by bicalutamide monotherapy of prostate cancer. J Clin Oncol. 2005; 23 (4): 808-15.
25. Plourde PV, Kulin HE, Santner SJ. Clomiphene in the treatment of adolescent gynecomastia. Clinical and endocrine studies. Am J Dis Child. Nov 1983; 137 (11): 1080-2.
26. Pensler JM, Long JN. Plastic Surgery for Gynecomastia Treatment & Management. Medscape Reference. 2014. http://emedicine.medscape.com/article/1273437-treatment#a1128.
27. “Coverage Determination Guideline”. United HealthCare Services, Inc. 2014. Effective Date: July 1, 2014. https://www.unitedhealthcareonline.com/ccmcontent/ProviderII/UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/Tools%20and%20Resources/Policies%20and%20Protocols/Medical%20Policies/Medical%20Policies/Gynecomastia_CD.pdf.
278 “Clinical Policy Bulletin: Breast Reduction Surgery.” Aetna Inc. 2014. Last Reviewed: September 12, 2014. http://www.aetna.com/cpb/medical/data/1_99/0017.html.
29. “Cigna Medical Coverage Policy”. Cigna. 2014. Effective Date: October 15, 2014. https://cignaforhcp.cigna.com/public/content/pdf/coveragePolicies/medical/mm_0195_coveragepositioncriteria_surgical_treatment_of_gynecomastia.pdf.
30. American Society of Plastic Surgeons. Male Breast Reduction Surgery Cost. 2013. http://www.plasticsurgery.org/cosmetic-procedures/gynecomastia-surgery.html?sub=Gynecomastia+surgery+cost.