In recent years, testosterone replacement therapy (TRT) for low testosterone has gained widespread interest from aging men and acceptance from the medical community. With an aging male population, less stigma, and more popular advertisement, more and more men are consulting with their physicians about testing for low testosterone and initiating TRT.
What is Testosterone Replacement Therapy?
Testosterone replacement therapy is the hormone treatment of testosterone prescribed by a physician to counter the effects of low testosterone. The following EMG Testosterone Section provides an in-depth review of TRT to make you a better-informed man. Here, you will learn about testosterone levels and aging, symptoms of low testosterone, as well as TRT benefits and side effects. Also, learn about different administration methods (including transdermal, injectable, implantable, transbuccal and oral forms) as well as ways to increase testosterone naturally. Select any link for a more in-depth discussion.
Page Table of Contents
- 1 ♦ Testosterone Levels By Age
- 2 ♦ Low Testosterone Diagnosis
- 3 ♦ Symptoms of Low Testosterone
- 4 ♦ Types of Testosterone
- 5 ♦ Benefits of Testosterone Replacement Therapy
- 6 ♦ Side Effects of Testosterone Replacement Therapy
- 7 ♦ How to Increase Testosterone Naturally
- 8 ♦ Testosterone Replacement Therapy and Fertility
♦ Testosterone Levels By Age
Why do some men end up with low testosterone? In men testosterone production slowly declines after early adulthood as part of the normal aging process. This decline continues throughout life. Even worse, free testosterone (the active form of testosterone not bound to sex hormone binding globulin (SHBG)) declines even more than total testosterone.1-3 Free testosterone is the free, active form of testosterone in the body. So, its decline may be even more important than the decline in total testosterone.
The official term for this decline is late onset hypogonadism (LOH) also known as andropause. It’s more commonly referred to as low testosterone or “low T”.
As a result of this slow progressive decline in testosterone, some men will have levels that fall below the normal total testosterone range (300 – 1050 ng/dL). Men with low testosterone and the associated symptoms may benefit from testosterone replacement therapy. (For more information, see EMG’s Testosterone Levels by Age and Sex Hormone Binding Globulin Articles).
♦ Low Testosterone Diagnosis
To determine whether or not you have low testosterone, a physician will request a blood test to measure your total testosterone level. This test may also measure your free testosterone and sex hormone binding globulin levels. Generally speaking, the cutoff range for low testosterone is a total testosterone level of less than 300 ng/dL with associated symptoms.4
However, no absolute consensus among different medical organizations exists for the exact cutoff value. The American Association of Clinical Endocrinologists suggests levels as low as 200 ng/dL as the cutoff,5 while the European Society of Urology suggests levels as high as 350 ng/dL.6 Another organization, the Japanese Urological Association, suggests that total testosterone not be used at all. Rather, this organization suggests that the diagnosis of low testosterone should be based solely off of free testosterone values.7
♦ Symptoms of Low Testosterone
Low testosterone can cause unwanted symptoms. It is important to be aware of these symptoms. If you have these symptoms, discuss them with your physician. Your doctor can perform simple blood tests to determine whether your testosterone levels are low or not. Additional tests of use include a measurement of LH (luteinizing hormone) levels, FSH (follicle stimulating hormone) levels, prolactin levels, and a full thyroid panel.
Symptoms of low testosterone may include:
- Decreased sex drive
- Erectile dysfunction
- Loss of muscle mass
- Reduced energy level
- Reduced strength and endurance levels
- Sleep problems
- Increased breast size and tenderness
- Decrease in amount of body hair
- Emotional instability
These symptoms may be caused by an unrelated issue, so experiencing one or more of these symptoms does not necessarily mean you have low T. Nonetheless, it is important to be aware of these potential symptoms and discuss them with your physician.
The ADAM Questionnaire also helps men decide if they should talk to their doctor about low testosterone. It consists of ten ‘yes or no’ questions about your health and well-being. While it is not use for diagnosis, it may help as a starting point in your discussions.
♦ Types of Testosterone
Testosterone replacement therapy involves the administration of testosterone. Testosterone most commonly comes in one of the following forms: 1) gels, 2) injections, 3) implants, or 4) lozenges. Each form possesses different time between applications, ease of administration, and potential for side effects. The most commonly prescribed forms are testosterone gels and injections.
The fundamental goal of treatment is to re-establish normal T levels. Other goals include re-establishing sexual function and libido and improving overall mood. Restoring testosterone to normal levels can also improve muscle mass, reduce fat mass, prevent osteoporosis, and maintain virilization, especially in older men.8 (For more information, see EMG’s Types of Testosterone Article).
- Testosterone Gel - Gels deliver testosterone through the skin. This form is the newest form of testosterone, so most options are available under a brand name. These include Androgel, Axiron, Bio-T-Gel, Fortesta, Testim, and Vogelxo.
- Testosterone Injections - Injectable testosterone delivers testosterone deep into the muscle via an injection. Over time, the testosterone is absorbed into the blood stream. Injections generally take place once per week. This form is the oldest form of testosterone, so most options are available as generics. These include testosterone cypionate, enanthate, and undecanoate (under the brand name Aveed).
- Testosterone Implants - Implants in the form of small pellets are implanted under the skin in the fat layer by your physician. They slowly deliver testosterone over the course of three to six months, so only two to four implants must be performed per year. Testopel is the only FDA approved implantable testosterone treatment on market.
- Testosterone Lozenges - Lozenges are placed under the tongue or against the surface of your gums twice daily. The lozenge is designed to adhere to the gum or inner check for a 12 hour period, after which time it is replaced. The only FDA approved transbuccal testosterone replacement product in the US is Striant.
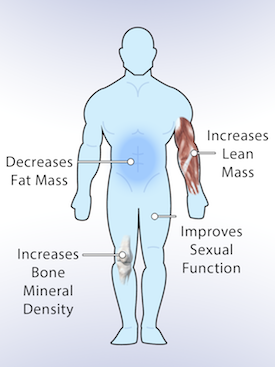
♦ Benefits of Testosterone Replacement Therapy
Testosterone replacement therapy in men has shown to produce numerous benefits with minimal side effects, and these benefits can be both physical and mental.
The following benefits may result by restoring testosterone levels via testosterone therapy to within the normal range:9-11
- Increase lean body mass
- Decrease fat mass
- Increase bone mineral density
- Improve sexual function
- Improve mood and well-being
Although some benefits appear in the first month of therapy, most effects begin to take place over the first few months. (For more information, see EMG’s Benefits of Testosterone Therapy Article).
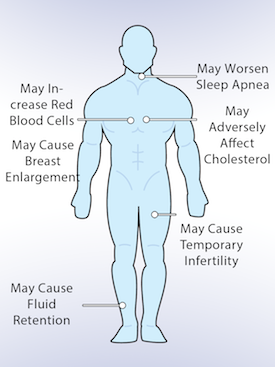
♦ Side Effects of Testosterone Replacement Therapy
Side effects of testosterone replacement therapy are generally minimal as long as testosterone is kept within the normal range. Like any prescription therapy, though, TRT can cause side effects. Side effects may include an increase in red blood cell count, worsening of sleep apnea, temporary infertility, breast enlargement, fluid retention, and negative changes to cholesterol.12-18 Certain conditions, like the existence of prostate cancer, breast cancer, or uncontrolled congestive heart failure may also prevent use.4
For years, physicians have worried that one of the potential side effects of testosterone replacement therapy would be the causing or worsening of prostate cancer. Fortunately, most studies agree that testosterone does not induce a development of malignant prostate cells.19-22 Also, testosterone therapy may increase the prostate’s size, but the evidence shows that it does not cause or worsen symptoms of BPH.23-24
Anyone considering TRT should be aware that as of January 31st, 2014, the U.S. FDA said that it is investigating the risk of stroke, heart attack, and death in men taking FDA-approved testosterone products based on the cited studies.25-26 (See EMG’s FDA Statement Regarding TRT Article). Subsequently, the FDA voted to require manufacturers of testosterone to change labeling to inform of possible increased risk of heart attack and stroke with use. (For more information, see EMG’s Side Effects of Testosterone Therapy Article).
Interestingly, a new meta-analysis (Testosterone Replacement Therapy and Cardiovascular Risk: Advances and Controversies) in the Mayo Clinic Proceedings published during this FDA review says there is no evidence of increased cardiovascular risks in its analysis. This meta-analysis is the largest to date, and it revealed no increase in cardiovascular risks in men who received testosterone. It also revealed reduced cardiovascular risk among those men with metabolic disease. This analysis contradicts the findings of the two studies that led the FDA to begin a review of the risk of cardiovascular disease in men taking testosterone therapy.27
♦ How to Increase Testosterone Naturally
As mentioned above, many men will never need testosterone replacement therapy. Additionally, many men will choose not to use it. Fortunately, certain healthy lifestyle choices, such as weight lifting, vigorous aerobic exercises, and proper diet, may actually increase testosterone production naturally. On the other hand, certain poor lifestyle choices, such as smoking and heavy drinking, may actually significantly decrease testosterone. (For more information, see EMG’s How to Increase Testosterone Naturally Article).
♦ Testosterone Replacement Therapy and Fertility
As mentioned above, one side effect of testosterone replacement therapy is temporary infertility. Testosterone therapy suppresses the natural production of testosterone by the testes, which also reduces sperm production. As a result, most men on TRT are infertile. As a note, infertility is usually reversible if the testosterone dosage is either decreased or TRT is stopped all together.15 While this side effect may not concern certain men, men looking to conceive a child or remain fertile must be aware of this potential side effect.
Fortunately, maintaining fertility may be accomplished by also taking human chorionic gonadotropin (HCG) during testosterone replacement therapy. Adding HCG to TRT may sustain continued sperm production necessary for conception in patients on testosterone therapy.28-29 (For more information, see EMG’s Human Chorionic Gonadotropin and Testosterone Therapy Article).
The Future of Testosterone Replacement Therapy and Andropause
It should be noted that there is not complete agreement on the threshold value of testosterone below which a man would be considered to have low testosterone. The wide normal testosterone range presents a major challenge in defining low testosterone levels. For young men, the accepted normal total level generally ranges from 300 ng/dL to 1050 ng/dL. This means that one man could have a level 2-3x higher than that of another man, while both are considered normal. There are indication that the threshold required for behavioral effects of testosterone increases with aging.30-31
Consequently, there are some interesting questions yet to be answered regarding the definition of low testosterone and the implementation of testosterone replacement therapy in men. These questions are as follows:
- Should the definition of a “low testosterone level” be different for older men?
- Should other criteria for testosterone deficiency be established for older men?
- Should the existence of clinical symptoms of low testosterone, despite a normal level, constitute a medical diagnosis by itself?
Ultimately, the diagnosis of low testosterone and the decision to pursue testosterone replacement therapy is typically considered on an individual basis rather than simply being based on numerical guidelines for generally accepted “normal” testosterone levels.
Read On
For those with low testosterone, combining proper diet and exercise and good sleep with testosterone replacement therapy can make you both stronger and leaner and feel better. Check out the links below to to explore The Elite Men’s Guide Exercise for Men, How to Eat Healthy: Good Nutrition and Importance of Sleep sections as well as EMG’s Health Numbers to know where you and your health numbers stand.
The following links provide the basics on testosterone. Also, check out the external resources. These resources provide the most authoritative information on testosterone.
- What is Testosterone? Where is it Produced?
- What Does Testosterone Do?
- Recent FDA Statement on Testosterone
External Resources:
- Medscape: Andropause
- Mayo Clinic: Testosterone Replacement Therapy
- Endocrine.org: Testosterone Therapy in Men
Updated: May 5, 2015
1. Moffat SD, Zonderman AB, Metter EJ, Blackman MR, Harman SM, Resnick SM. Longitudinal assessment of serum free testosterone concentration predicts memory performance and cognitive status in elderly men. J Clin Endocrinol Metab. 2002; 87 (11): 5001-5007.
2. Morley JE, Kaiser FE, Perry HM, et al. Longitudinal changes in testosterone, luteinizing hormone, and follicle-stimulating hormone in healthy older men. Metabolism. 1997; 46 (4): 410-413.
3. Araujo AB, O’Donnell AB, Brambilla DJ, et al. Prevalence and incidence of androgen deficiency in middle-aged and older men: estimates from the Massachusetts Male Aging Study. J Clin Endocrinol Metab. 2004; 89 (12): 5920-5926.
4. Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Synder PJ, Swerdloff RS, Montori, VM. Testosterone replacement therapy in men with androgen deficiency syndromes: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2010, 95 (6): 2536–2559.
5. Anderson RJ, Bergman DA, Garber JR, Hamilton CR, Hershon KS, Jovanovic LG, Kleerekoper M, Mechanick JI, Palumbo PJ, Peters AL, Rettinger HI, Rodbard HW, Rubenstein HA, Seibel JA, Tourtelot JB. American association of clinical endocrinologists medical guidelines for clinical practice for the evaluation and treatment of hypogonadism in adult male patients. AACE Hypogonadism Guidelines, Endocr Pract. 2002; 8 (6): 439-456.
6. Wang C, Nieschlag E, Swerdloff R, Behre HM, Hellstrom WJ, Gooren LG, Kaufman JM, Legros JJ, Lunenfeld B, Morales A, Morley JE, Schulman C, Thompson IM, Weidner W, and Wu FCW. Investigation, treatment and monitoring of late-onset hypogonadism in males ISA, ISSAM, EAU, EAA and ASA recommendations. Eur J Endocrinol. 2008 Nov; 159(5): 507–514.
7. Namiki M, Akaza H, Shimazui T, Ito N, Iwamoto T, Baba K, Kumano H, Koh E, Tsujimura A, Matsumiya K, Horie S, Maruyama O, Marumo K, Yanase T, Kumamoto Y. Clinical Practice Manual for Late-onset Hypogonadism Syndrome. International Journal of Urology. 2008; 15 (5): 377-388.
8. Ohl DA, Quallich, SA. Clinical Hypogonadism (Andropause) and Androgen Replacement Therapy: An Overview. Urol Nurs. 2006; 26(4):253-259, 269.
9. Ferrando AA, Sheffield-Moore M, Yeckel CW, et al. Testosterone administration to older men improves muscle function: molecular and physiological mechanisms. Am J Physiol Endocrinol Metab. 2002; 282 (3): E601-607.
10. Rolf C, von Eckardstein S, Koken U, Nieschlag E. Testosterone substitution of hypogonadal men prevents the age-dependent increases in body mass index, body fat and leptin seen in healthy ageing men: results of a cross-sectional study. Eur J Endocrinol. 2002; 146 (4): 505-511.
11. Amory JK, Watts NB, Easley KA, et al. Exogenous testosterone or testosterone with finasteride increases bone mineral density in older men with low serum levels. J Clin Endocrinol Metab. 2004; 89 (2): 503-510.
12. Claustres M, Sultan C. Androgen and erythropoiesis: evidence for an androgen receptor in erythroblasts from human bone marrow cultures. Horm Res. 1988; 29 (1): 17-22.
13. Drinka PJ, Jochen AL, Cuisinier M, Bloom R, Rudman I, Rudman D. Polycythemia as a complication of testosterone replacement therapy in nursing home men with low levels. J Am Geriatr Soc. 1995; 43 (8): 899-901.
14. Jockenhövel F, Vogel E, Reinhardt W, Reinwein D. Effects of various modes of androgen substitution therapy on erythropoiesis. Eur J Med Res. 1997; 2 (7): 293-298.
15. Miner MM. Low Testosterone Medscape CME Expert Column Series. Issue 3: Delivering Safe and Effective Testosterone Replacement Therapy. Medscape Education. 2011.
16. Sandblom RE, Matsumoto AM, Schoene RB, et al. Obstructive sleep apnea syndrome induced by testosterone administration. N Engl J Med. 1983; 308 (9): 508-510.
17. Schneider BK, Pickett CK, Zwillich CW, et al. Influence of testosterone on breathing during sleep. J Appl Physiol. 1986; 61 (2): 618-623.
18. Liu PY, Yee B, Wishart SM, et al. The short-term effects of high-dose testosterone on sleep, breathing, and function in older men. J Clin Endocrinol Metab. 2003; 88 (8): 3605-3613.
19. Carter HB, Pearson JD, Metter EJ, et al. Longitudinal evaluation of serum androgen levels in men with and without prostate cancer. Prostate. 1995; 27 (1): 25-31.
20. Slater S, Oliver RT. Testosterone: its role in development of prostate cancer and potential risk from use as hormone replacement therapy. Drugs Aging. 2000; 17 (6): 431-439.
21. Heikkilä R, Aho K, Heliövaara M, et al. Serum testosterone and sex hormone-binding globulin concentrations and the risk of prostate carcinoma: a longitudinal study. Cancer. 1999; 86 (2): 312-315.
22. Hsing AW. Hormones and prostate cancer: what’s next? Epidemiol Rev. 2001; 23 (1): 42-58.
23. Behre HM, Bohmeyer J, Nieschlag E. Prostate volume in testosterone-treated and untreated hypogonadal men in comparison to age-matched normal controls. Clin Endocrinol (Oxf). 1994; 40 (3): 341-349.
24. Jin B, Conway AJ, Handelsman DJ. Effects of androgen deficiency and replacement on prostate zonal volumes. Clin Endocrinol (Oxf). 2001; 54 (4): 437-445.
25. Vigen R, O’Donnell CI, Baron AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013; 310 (17): 1829-1836.
26. Finkle, WD, Hoover, RN, et al. Increased Risk of Non-Fatal Myocardial Infarction Following Testosterone Therapy Prescription in Men. PONE. January 29, 2014.
27. Morgentaler A, Miner MM, Caliber M, Guay AT, Khera M, Traish AM. Testosterone replacement therapy and cardiovascular risk: advances and controversies. Mayo Clinic Proceedings. 2015; 90 (2): 224-251.
28. Coviello AD, Matsumoto AM, Bremner WJ, Herbst KL, AmoryJK, Anawalt BD, Sutton PR, Wright WW, Brown TR, Yan X, Zirkin BR, Jarow JP. Low-Dose Human Chorionic Gonadotropin Maintains Intratesticular Testosterone in Normal Men with Testosterone-Induced Gonadotropin Suppression. J Clin Endrocrinol and Metab. 2005. 90 (5): 2595–2602.
29. Hsieh TC, Pastuszak AW, Hwang K, Lipshultz LI. Concomitant intramuscular human chorionic gonadotropin preserves spermatogenesis in men undergoing testosterone replacement therapy. J Urol. 2013. 189 (2): 647-50.
30. Schiavi RC, Rehman J. Sexuality and aging. Urol Clin. North Am. 1995; 22: 711-726.
31. Gray PB, Singh AB, Woodhouse LJ et al. Does-dependent effects of testosterone on sexual function, mood, and visuospatial cognition in older men. J. Clin. Endocrinol. Metab. 2005; 90: 3838-3846.